Pulmonary embolism: what you need to know
Introduction: Why pulmonary embolism matters
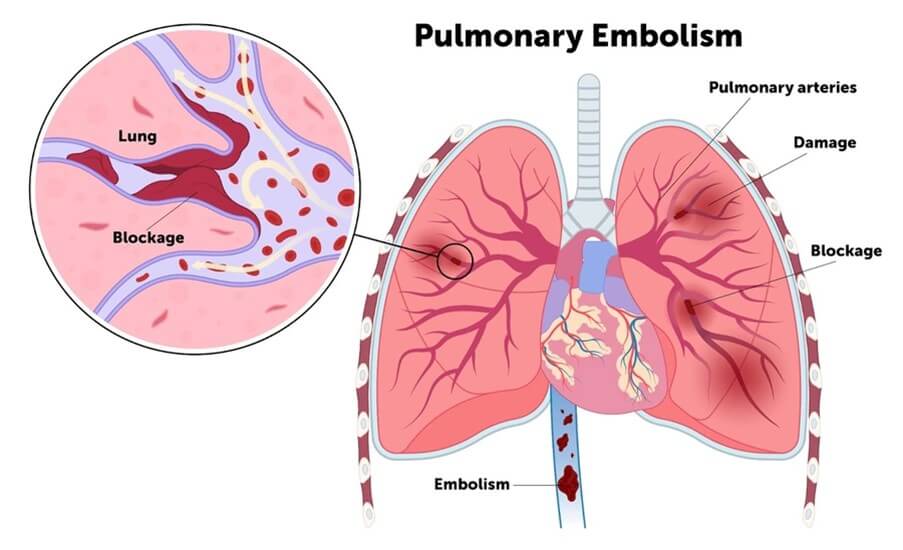
Pulmonary embolism (PE) is a potentially life‑threatening blockage of the lung arteries, most commonly caused by a blood clot that has travelled from the leg (deep vein thrombosis). PE is a major public‑health concern: it is a common form of venous thromboembolism and a leading acute cardiovascular cause of death. Timely recognition, diagnosis and treatment substantially reduce the risk of severe complications and mortality, so public and clinical awareness is crucial.
Main body: causes, signs, diagnosis and treatment
Causes and risk factors
Most PEs arise from clots in the deep veins of the legs or pelvis. Risk factors include recent surgery or trauma, prolonged immobility (for example long flights or hospital stays), active cancer, pregnancy and the postpartum period, hormone replacement therapy or combined oral contraceptives, inherited thrombophilias, obesity and older age. A significant proportion of cases are provoked by a clear trigger; however, some occur without an obvious cause.
Typical symptoms and warning signs
Symptoms can vary from mild breathlessness to sudden collapse. Common features are sudden onset shortness of breath, pleuritic chest pain (worse on breathing), fast heart rate, light‑headedness or fainting, cough and sometimes coughing up blood (haemoptysis). Symptoms can be subtle, particularly in older people, so any unexplained new breathlessness should prompt medical assessment.
Diagnosis and assessment
Assessment begins with clinical evaluation and risk stratification. Blood tests such as D‑dimer are useful to rule out PE in low‑risk patients. Imaging is required to confirm the diagnosis: computed tomography pulmonary angiography (CTPA) is the preferred test in most settings; ventilation–perfusion (V/Q) scanning is an alternative in selected patients. Lower limb ultrasound can identify a source clot. Electrocardiography and blood gas analysis provide supportive information but are not diagnostic.
Treatment and prevention
Immediate anticoagulation is the mainstay of treatment to prevent clot growth and new events. Options include low‑molecular‑weight heparin and direct oral anticoagulants, with thrombolysis reserved for high‑risk (massive) PE and surgical or catheter embolectomy for selected cases. Preventive measures—early mobilisation after surgery, mechanical compression and pharmacological prophylaxis—are effective in reducing risk.
Conclusion: implications for readers
Pulmonary embolism is a common, potentially fatal condition that responds well to prompt diagnosis and treatment. Recognising symptoms early, understanding personal risk factors and following preventive advice around surgery, travel and immobility can reduce risk. Anyone with sudden unexplained breathlessness or chest pain should seek urgent medical assessment.








